View Phases
Criteria to be in place before relaxing social distancing orders within the community.
Infection Rate: Infection rates should be declining, with each case infecting less than 1.00 person (R0 < 1 and approaching 0). Percent positive of diagnostic tests conducted should be consistently low.
Diagnostic test positivity rate [without testing restrictions]
- Phase 2: <10% of tests conducted are positive for COVID-19
- Phase 3: <3% of tests conducted are positive for COVID-19
- Phase 4: <1% of tests conducted are positive for COVID-19
Overall case count
- All Phases: Sustained decline in daily case counts for 21 consecutive days, as reflected in the 5-day rolling average.
- Phase 2: <25 new cases/100,000 population per day, with widespread testing
- Phase 3: <10 new case/100,000 population per day, with widespread testing
- Phase 4: <1 new case/100,000 population per week, with widespread testing
Community Diagnostic Testing and Surveillance: Community surveillance is able to rapidly identify all new cases. Diagnostic testing for active infections is rapidly and widely available to all who seek it.
Diagnostic Testing Rate
- Phase 2: Increasing number of tests per day per 100,000 population, using this tool or similar.
- Phase 3: Increasing number of tests per day (nearing sufficiency), per day per 100,000 population, using this tool or similar.
- Phase 4: Sufficient number of tests per day per 100,000 population, using this tool or similar.
Availability of Diagnostic Testing
- Phase 2: All symptomatic people regardless of severity, and all asymptomatic high-risk individuals or contacts, regardless of severity, can access testing and obtain a result within 48 hours of request.
- Phase 3: All symptomatic people regardless of severity, and all asymptomatic high-risk individuals or contacts, can access testing and obtain a result within 24 hours of request.
- Phase 4: All symptomatic people regardless of severity, all asymptomatic high-risk individuals or contacts, and anyone who requests a test/any physician who orders a test can access testing and obtain a result within 24 hours of request.
Timeliness of Diagnostic Testing
- Phase 2: Majority of tests results are returned within 48 hours
- Phase 3 and 4: Majority of tests results are returned within 24 hours.
Availability of Diagnostic Testing for Healthcare Workers and Others at Greater Risk
- Phase 2: Majority of healthcare workers, first responders, critical infrastructure employees, and others at greater risk can access testing once per week, whether or not they are experiencing symptoms.
- Phase 3: Majority of healthcare workers, first responders, critical infrastructure employees, and others at greater risk can be tested at least once per week, whether or not they are experiencing symptoms.
- Phase 4: Majority of healthcare workers, first responders, critical infrastructure employees, and others at greater risk can be tested every 2-3 days, whether or not they are experiencing symptoms.
*Antibody tests can be instituted when more is known regarding accuracy.
Community Syndromic Surveillance and Diagnostic Testing
- All Phases: The community is conducting syndromic surveillance for increases in influenza-like illness ILI-like or COVID-19- like illness.
- All Phases: Sentinel surveillance through widespread testing is underway in long-term care facilities, prisons, detention centers, shelters, high-risk workplaces, and other high-risk settings.
- All Phases: Testing supplies (swabs, viral transport media), reagents, equipment, staffing, and laboratory processing capacity are sufficient to meet the above metrics - without rationing.
Case and Contact Investigations: Capacity to rapidly and efficiently isolate those with COVID-19, provide case management services, and identify and quarantine their contacts.
Workforce Availability
- All phases: At least 30 trained contact tracers are available for case management and health education per 100,000 population*
*Programs may need to adjust recruitment depending on caseload and contact load per tracer. - All phases: Sufficient community health workers, case management, care resource coordinators, and health education is available.
- All phases: Percentage of contacts reached relative to number of contacts elicited.
Effectiveness of Contact Tracing
- Phase 2: At least 60% of new cases are coming from among identified contacts, with a steady or increasing percentage of cases captured over time.
- Phase 3: At least 80% of new cases are coming from among identified contacts, with a steady or increasing percentage of cases captured over time.
- Phase 4: At least 90% of new cases are coming from among identified contacts.
Rapidity of testing contacts for people with positive diagnostic test results and people experiencing ILI or COVID-19-like illness
- Phase 2: At least 75% of contacts are elicited, located, and placed under quarantine within 48 hours of case identification.
- Phase 3: At least 90% of contacts are elicited, located, quarantined, and tested within 24 hours of case identification.
- Phase 4: At least 95% of contacts are elicited, located, quarantined, and tested within 24 hours of case identification.
Availability of safe isolation and quarantine facilities
- All Phases: Safe isolation and quarantine facilities, as well as support services, are available for those in need, especially for all testing positive and their close contacts.
- Phase 3: 25-33% of isolation and quarantine stays are successfully completed.
- Phase 4: 50-60% of isolation and quarantine stays are successfully completed.
Case Management
- All Phases: 100% of contact tracers within the community are using a unified system for case management, which securely logs and reports contacts to the health department in real time.
- All Phases: Two or more outbreaks reported a week of non-household cases (in a workplace, congregate living, or institutional setting) and epidemiologically linked within 14 days.
Healthcare System and Hospital Readiness: Adequate bed capacity, PPE, equipment, staffing, and supplies are in place to handle surge in COVID-19 cases without resorting to crisis standards of care.
Availability of ICU Capacity and Staffing for Surge of COVID-19 Patients
- Phase 2: At least 15% of existing ICU capacity is available to accommodate a surge in COVID-19 patients.
- Phase 3 and 4: At least 30% of existing ICU or other surge capacity is available to accommodate a surge in COVID-19 patients.
- All Phases: Surge capacity - either a designated site or within each hospital system - exists to handle a 20% surge in COVID-19 cases without resorting to crisis standards of care.
Ability of Hospitals to Coordinate the Movement of Patients to Support a Surge of COVID-19 Cases Without Using Crisis Standards of Care
- All Phases: Hospitals are able to surge and coordinate the movement of patients to support a surge of COVID-19 cases without using crisis standards of care.
Availability of Personal Protective and Medical Equipment: Sufficient PPE and medical equipment is available to support a surge in COVID-19 cases without resorting to crisis standards of care
Availability of PPE in Healthcare Settings
- All Phases: PPE is available for all essential personnel, critical infrastructure employees, and staff of high-risk facilities.
- Phase 2: The majority of hospitals, long-term care facilities, homeless shelters, and other healthcare settings report sufficient PPE to treat COVID-19 patients and protect healthcare workers.
- Phase 3: 100% of hospitals, long-term care facilities, homeless shelters, and other healthcare settings report sufficient PPE to treat COVID-19 patients, conduct daily operations, and protect and protect healthcare workers. Reserve of PPE stockpiled for at least 2-4 weeks.
- Phase 4: 100% of hospitals, long-term care facilities, homeless shelters, and other healthcare settings report sufficient PPE to treat COVID-19 patients, conduct daily operations, and protect and protect healthcare workers. Reserve of PPE stockpiled for at least 90 days.
Availability of PPE for Emergency Management Agencies and Essential Services Providers
- All Phases: High priority PPE requests are always fulfilled for local emergency management agencies.
- Phase 2: PPE is available for all essential personnel and critical infrastructure employees, and staff of high-risk facilities.
- Phase 3 and 4: PPE is available for all essential personnel, critical infrastructure employees, staff of high-risk facilities, and additional employees who require PPE to be safe in a work environment.
Availability of Lifesaving Medical Equipment in Healthcare Settings
- Phase 2: Majority of hospitals treating COVID-19 patients report sufficient ventilators, oxygen, supplies, and healthcare workers required to support intubation of all COVID-19 patients as needed.
- Phase 3 and 4: 100% of hospitals treating COVID-19 patients report sufficient ventilators, oxygen, supplies, and healthcare workers required to support intubation of all COVID-19 patients as needed.
Protecting At-Risk Populations
Cases in At-Risk Facilities
- All Phases: Sufficient testing and quarantine/isolation capacity is available in long-term care facilities.
- Phase 2: Percentage of cases reported from long-term care facilities is less than 20% over the last 28 days.
- Phase 3: Percentage of cases reported from long-term care facilities is less than 10% over the last 28 days.
- Phase 4: Percentage of cases reported from long-term care facilities is less than 5% over the last 28 days.
Rapid Response Teams
- All Phases: Local rapid response teams are available to respond to outbreak hotpots within 24 hours and have sufficient PPE for localized outbreak response.
Sentinel Surveillance
- All Phases: Sentinel surveillance and testing sites are operating in long-term care facilities and other locations serving older individuals, lower-income individuals, and racial and ethnic minorities including Native Americans.
Availability of PPE
- All Phases: The majority of long-term care facilities and homeless shelters have sufficient PPE available.
- All Phases: State and local rapid response teams have sufficient PPE for localized outbreak response.
Communication and Adherence to Social Distancing
Communication surrounding social distancing
- All Phases: Adequate communications methods are in place to deliver information, including in at-risk communities (e.g. homeless, immigrant, low-income populations.)
- All Phases: The majority of residents are knowledgeable about restrictions.
Adherence to social distancing
- All Phases: The majority of the community is adhering to social distancing requirements.
Progress: Phase 2: 0%
Phase 3: 0%
Phase 4: 0%
Activation of an emergency operations center (EOC) with an incident command structure to manage local response efforts.
Is there a clearly designated and empowered incident manager?
Are there clearly designated organizational units in the EOC aligned with principal operational priorities (e.g., testing, hospital capacity, crisis communication, protection of high-risk populations, etc)?
Community is able to rapidly identify all infected individuals, isolate them, and quickly and effectively quarantine and trace their contacts.
Is the percentage of positive diagnostic tests relative to the total number of tests declining, and is that number low enough (e.g. 3 %) to indicate your testing is identifying most cases?
Are most new cases from identified contacts?
Are accurate diagnostic tests broadly available in the community with timely results (e.g. 24 hours)?
Have contract tracing teams been trained?
Have contact tracing teams been deployed sufficient to meet demand (e.g. 5 tracers for each positive case)?
Are there specific, interoperable methods deployed in your community for obtaining and managing data collection and integration for diagnostic testing and tracing?
Availability and accessibility of COVID-19 diagnostic testing throughout the community.
Is COVID-19 diagnostic testing available to all experiencing symptoms within 24 hours? n the community meeting medical demand?
Are COVID-19 diagnostic test results returned within 24 hours?
Can healthcare workers, first responders, essential service providers, and those at greater risk, always access COVID-19 diagnostic testing, whether or not they are experiencing symptoms?
Can healthcare workers, first responders, others at high-risk, be regularly tested (e.g. every 2-3 days), whether or not they are experiencing symptoms?
Are there shortages in the diagnostic testing supply chain–including equipment, supplies, reagents, and staffing?
Are serological (antibody), as well as diagnostic tests available?
Existence of an accurate understanding of the COVID-19 transmission trend within your community.
Do you have an accurate understanding of the level of COVID-19 transmission?
Does the general public in your community have an accurate understanding of the status of COVID-19 transmission through daily updates?
Implementation of Infection, Prevention, and Control Measures to Prevent Disruptions in Critical Services, including:
Food supply and distribution?
Critical infrastructure?
Water supply?
Waste management?
Electricity?
Institute protective measures for facilities serving high-risk populations.
Has a comprehensive list of facilities that house high-risk populations been compiled?
Have those facilities’ infection prevention and hygiene practices been assessed and verified?
Have all identified vulnerabilities at those facilities been addressed?
Availability of critical care/intensive care treatment capacity in your area.
Are you able to project approximate anticipated bed needs over the next 2 weeks?
Are the hospitals in your community able to meet current and projected demand for critical care/intensive care unit capacity?
Are you implementing measures to expand critical care/intensive care unit capacity?
Are local health care facilities separating intake for patients with COVID-19, or who may have COVID-19, from those needing other types of care?
Sufficient and Available Supply of Personal Protective Equipment (PPE) for:
Critical care units?
Testing centers?
Assisted living centers and other facilities housing high-risk populations?
EMTs and other frontline responders?
Emergency management agencies, EMTs and other frontline responders?
State and local strike teams for localized outbreak response?
Implementation of a crisis communication strategy, including scheduled updates and clear lines of communication with critical stakeholders.
Progress: 0%
KEY OBJECTIVE #1
Activate an Emergency Operations Center and establish a whole-of-community incident management structure
Controlling a pandemic outbreak is a multi-disciplinary and whole-of-society endeavor, and the leadership and management structure must reflect that. Activating an Emergency Operations Center, as would occur in a natural disaster or other homeland security crisis, is a best practice used in previous large-scale novel outbreaks. The EOC should host a whole-of-community incident management structure, drawing on existing local emergency response plans and capacities where possible. Using an EOC enables a community to streamline communication, planning, decision-making, and operational coordination across a wide range of community leaders and stakeholders, including communication and alignment with higher-level (state/federal) EOC processes and decision cycles. The EOC should also have liaisons to, or representatives from, other levels of government, public health officials, civil society, religious leaders, the business community, academia, and others.
- Activate local Emergency Operations Center and connect to state/federal EOCs
- Designate an empowered Incident Manager
- Organize EOC functional units/teams around major operational priorities
- Establish liaisons to key government partners (state, federal) and community stakeholders
- Has the Emergency Operations Center (EOC) been activated and has the whole-of-community incident management structure been established? [1] [2] [3]
- Have functional teams in the EOC been organized around defined operational priorities (such as the key actions identified in this guide)? [2] [3]
- Does the EOC have designated liaisons with all relevant government, community, and private sector stakeholders, including: [1]
[2]
[3]
- Other state, local, and federal officials involved in the response?
- Healthcare coalitions, including hospitals, public health, EMS and other key elements of the health and medical sector?
- Civil society groups, religious institutions, and other community leaders?
- Appropriate representation from all departments and agencies?
- Has the EOC identified the critical workers/sectors in the community (healthcare, utilities, transport, food supply, etc.)?
- Is there a process to maintain the health and wellbeing of personnel assigned to work in the EOC?
[4]
- As quarantines and self-isolation requirements expand, is there a clear process for transitioning to a virtual EOC for non-essential personnel who still need to be engaged, as well as identifying alternates for those who may be infected?
- Has a response coordinator been designated and do they have the authority to:
[2]
[3]
- Bring issues directly to leadership for rapid resolution?
- Link with scientific and health experts to provide guidance based on the latest research?
- Is there a Continuity of Government plan to ensure continued essential services? (Example Here)
- Do essential businesses such as healthcare facilities or facilities serving vulnerable populations have continuity plans to ensure continued service?
- Is there a clearly delineated process by which health and medical stakeholders advance resource requests to the jurisdictional EOC?
- What key communications systems and technologies are needed in your EOC?
- Is there a plan in place to build and maintain over a prolonged period a common operating picture to share situational awareness with all key partners?
- What declarations or legal/regulatory guidance has been implemented and how do they impact the decisions that need to be made?
- Is there a process in place to ensure that timely, accurate risk communications are available and coordinated with all jurisdictional agencies?
- Are public health information specialists integrated into the Joint Information System?
- Have key stakeholders shared their continuity/contingency plans with the EOC?
- Do personnel need refresher training on Incident Command System (ICS) concepts?
- Has the EOC planned for potential attrition of first responders by establishing a continuity of operations plan to replace and supplement critical personnel?
PRIORITY ACTIONS
OPERATIONAL REQUIREMENTS
RESOURCES
National Response Framework, Fourth Edition Incident Command System Primer for Public Health and Medical Professionals: Appendix B: Incident Command System Primer for Public Health and Medical Professionals ICS Organizational Structure and Elements (FEMA) Incident Action Planning Process “The Planning P” Standardized Reporting Forms Framework for a Public Health Emergency Operations Centre EOC Skillsets User Guide • What Is an Incident Action Plan? National Incident Management System: ICS Resource Center FEMA LifeLines Surge Capacity Logistics 2017-2022 Health Care Preparedness and Response CapabilitiesKEY OBJECTIVE #2
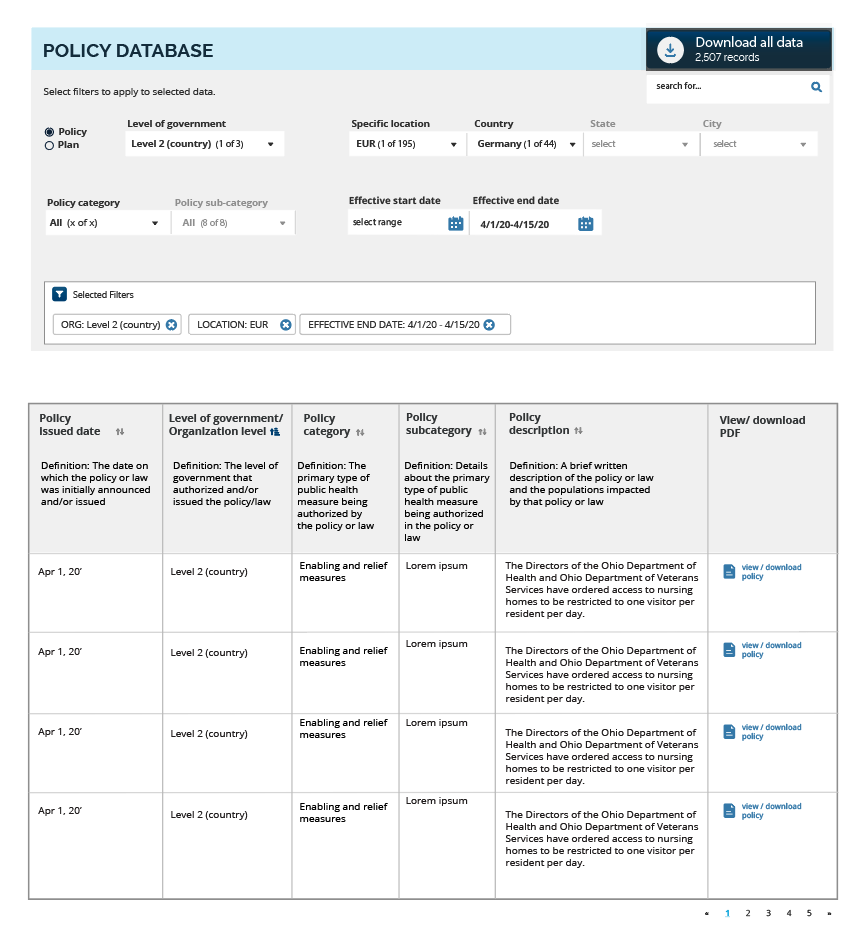
Understand and contain the real-time spread of COVID-19 in the community through surveillance, testing, contact tracing, and case quarantine and isolation
A pandemic control strategy is grounded in understanding ongoing transmission risk in the community so that the disease can be effectively controlled and contained. This will require continuous disease surveillance, diagnostic testing, contact tracing, isolation, and reporting systems that ensure up-to-date information on local spread is available to inform strategy-setting and daily tactical decision-making. This may be difficult where limited testing supplies and/or shortages of personal protective equipment prevent sufficient testing. Scaling up and sustaining local access to testing will be critical as additional laboratory capacity comes online. If diagnostic testing is limited, as a stop-gap, communities can enhance syndromic surveillance and other dynamic surveillance tools, along with contact tracing, to gauge disease activity within the community. Effective testing and contact tracing will require a combination of rapid testing capability, interoperable tools for quickly collecting and analyzing contract tracing data, deployment and management of contact tracing teams, and the provision of adequate capacity and incentives for the effective quarantine of contacts and isolation of infected persons. Contact tracing and testing must also be deployed in concert with other elements of a long term plan to contain and maintain control of community transmission. Other components include iterative cycles of social distancing measures –such as canceling mass gatherings, school closures, incentives for teleworking -- and expansion of health care capacity to meet the need.
- Does the community have clear plans, with metrics, for implementing, continuing, adjusting, or lifting social distancing measures incorporate benchmarks based on surveillance, testing, and contact tracing?
- Track influenza-like-illness (ILI) and COVID-19-like illness (CLI)
- Develop a protocol for broad diagnostic testing in the community. If tests are limited, include all symptomatic persons, close contacts, healthcare workers, first responders, essential service providers, and other at-risk individuals
- Develop a protocol for regular testing of healthcare workers, first responders and critical infrastructure employees
- Develop sentinel surveillance and testing sites in at-risk locations serving older individuals, lower-income individuals, racial and ethnic minorities including Native Americans
- Link COVID-19 testing and surveillance data to the local EOC
- Identify, hire, and train contact tracing workforce
- Develop a plan for follow up on positive tests including recommendations for isolation and treatment
- Identify and deploy a unified platform for entering cases and integrating any other technologies and data collected for contact tracing
- Identify capacity for quarantine and isolation of all contacts for positive and symptomatic cases, including for those who should be separated from other household contacts and those who are currently in long-term care settings, prisons, or are currently homeless
- Conduct and document formal risk assessment based on current level and trajectory of COVID-19 spread in the community
- Does the community have clear plans, with metrics, for implementing, continuing, adjusting, or lifting social distancing measures incorporate benchmarks based on surveillance, testing, and contact tracing? [1] [2] [3]
- Does the EOC have an accurate real-time picture of the trajectory of the outbreak within the community? [5] [6]
- Are health care providers in the area analyzing syndromic data on Influenza-Like Illnesses and Severe Acute Respiratory Illnesses as a proxy for COVID19?
- Is testing widely available for all those who need it, including all with symptoms, at high-risk, and those who are close contacts of infected persons?
[12]
[13]
- Are test results returned rapidly (24 hours)?
- Is same-day, point-of-care testing available for all patients exhibiting COVID-19 symptoms? Including:
[14]
[15]
- Hospitalized patients?
- Health care workers, first responders, essential service providers, and others in at-risk settings such as long-term care facilities?
- People who have had contact with infected persons (positive test or symptomatic person)?
- Symptomatic persons in outpatient settings (such as doctors’ offices)?
- Are sufficient test kits available?
- Have an overview of the supply chain for test kits, laboratory capacity to conduct testing, supplies (e.g. nasal swabs, test reagents) been conducted?
- Is there a plan and a specific timeline to fill identified gaps?
- Is guidance available for how to follow-up with and treat those who test positive?
[15]
[16]
[17]
- Is there a reporting structure to ensure medical providers are rapidly notified of results and have a clear plan to communicate to patients?
- Is data being reported up the chain from health care facilities/testing sites to local health officials? From local officials to both State and/or Federal officials?
- Are sentinel testing sites operating in locations serving older individuals, lower-income individuals, racial and ethnic minorities including Native Americans? [18]
- Has serological testing been incorporated to begin to determine how many people may have been exposed? [19]
- Have laboratory testing priorities been established and are they being implemented?
[20]
- Is there a lag time for receiving laboratory and clinical data? Have actions been identified and implemented to reduce the lag?
- Are there localized trade-offs between using scarce PPE for testing vs. treatment or other priorities? [21]
- Has a cadre of contact tracers been hired, trained, and deployed with the ability to trace most cases in the community?
[20]
- Has long-term funding been identified for contact tracing staff?
- Do training materials and implementation plans for contact tracers include actions and requirements associated with:
- Testing?
- Investigation and elicitation?
- Tracing?
- Quarantine or isolation?
- Follow-up?
- Is there a system in place to support data collection and tracking of contact tracing efforts available to the tracing teams?
- If technological or data collection tools are being used, have security requirements been defined and are protocols in place to ensure privacy and security of the data?
- Is there a system in place to support data collection and tracking of contact tracing efforts available to the tracing teams?
- Is there a plan in place to follow up with inbound travelers to assess their COVID-19 status and to provide guidance on self-isolation or quarantine, as needed? [32] [33]
- Have public messaging and communication efforts been updated to include contact tracing and testing guidance? [34] [35] [27] [29]
- Can the EOC receive notice of all cases tested in the community from both public and private health facilities? Is data disaggregated by:
[36]
[37]
- Vulnerable population status?
- Sex?
- Age?
- Healthcare worker status?
- Underlying condition status?
- Are public health personnel being redirected to highest yield interventions as case counts grow?
- Is there a method to assess the effectiveness of inbound traveler screening, taking into account the resources required?
PRIORITY ACTIONS
OPERATIONAL REQUIREMENTS
Surveillance: Is the community conducting active surveillance for COVID-19? Has a comprehensive surveillance system been implemented to monitor new cases in the community? [4]
Widespread, Rapid Testing: Can testing in your community fully meet medical demand and wider public demand? [7] [8] [9] [10] [11]
Contact Tracing: Is the public health workforce conducting contact tracing and monitoring of close contacts for confirmed cases? [17] [22] [23] [24] [25] [26] [27] [28] [29]
Quarantine and Isolation: Are there housing options available for those requiring quarantine, but who cannot be at home? [30] [31]
RESOURCES
Contact Tracing: Part of a Multipronged Approach to Fight the COVID-19 Pandemic Digital Contact Tracing Tools for COVID-19 Protocol to Investigate non-seasonal influenza and other emerging acute respiratory diseases, Annex 4: Contact tracing and monitoring procedures Protocol to Investigate non-seasonal influenza and other emerging acute respiratory diseases, Annex 4: Contact tracing and monitoring procedures Introduction to Public Health Surveillance Principles of Epidemiology in Public Health Practice, Third Edition an Introduction to Applied Epidemiology and Biostatistics. Lesson 6: Investigating an Outbreak Framework for a Public Health Emergency Operations Centre World Health Organization Surveillance Technical Guidance(note: includes a template for epi line listings)
World Health Organization Global COVID-19 Clinical Characterization Case Record Form and new data platform for anonymized COVID-19 clinical data(note: cities do not need to enroll, but this resource includes a checklist of key COVID-19 epi considerations)
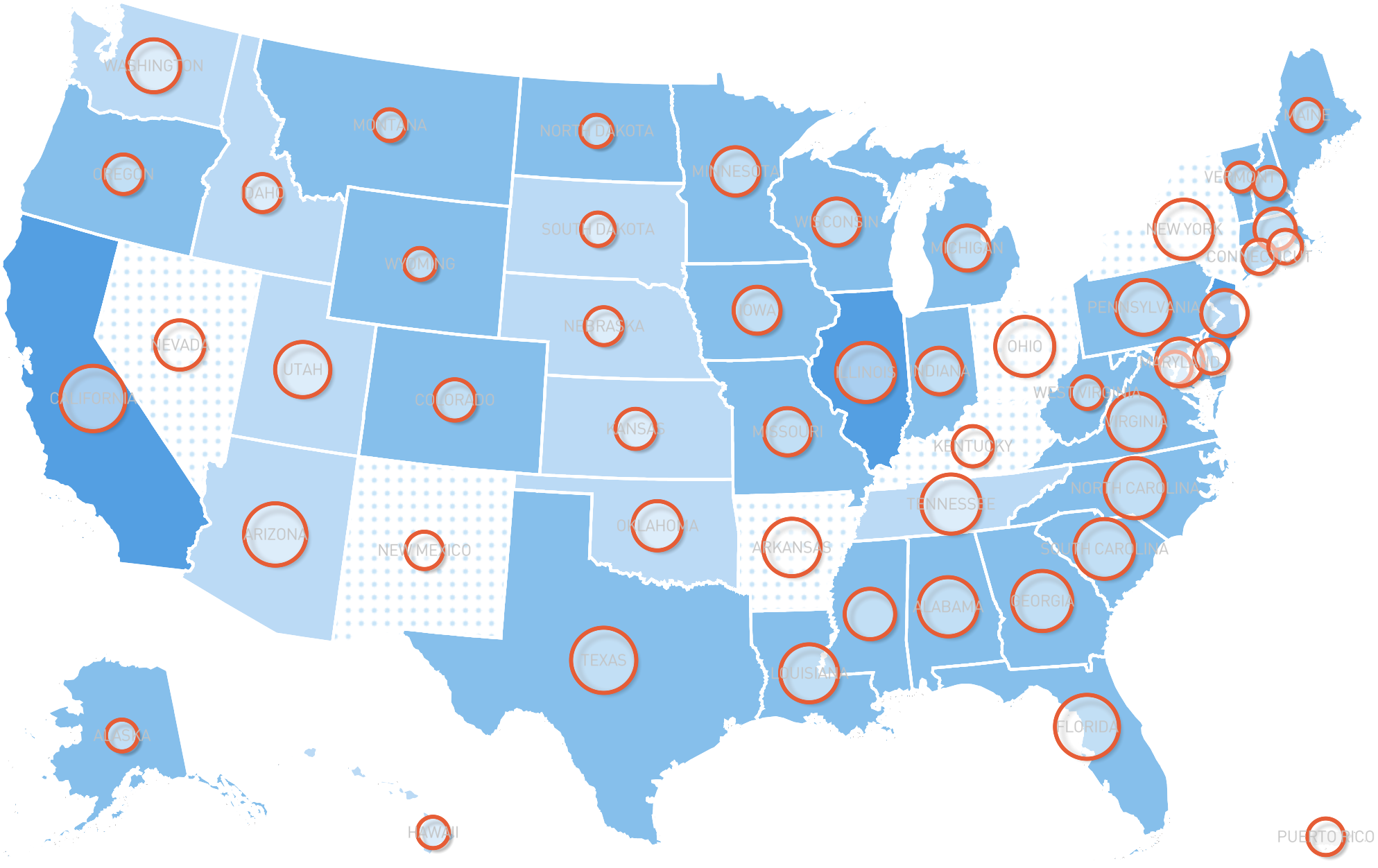
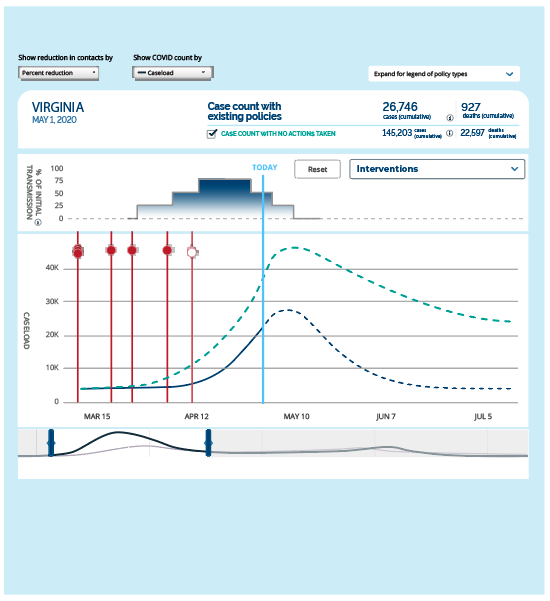
Fever Screening Continuity of Government - 2020 Contact Investigation (Airport) Reporting a PUI or Confirmed Case A Coordinated, National Approach to Scaling Public Health Capacity for Contact Tracing and Disease Investigation Making Contact: A Training for COVID-19 Contact Tracers Public Health Recommendations for Community-Related Exposure US CDC COVID-19 Contact Tracing Training Guidance and Resources Example Framework: Community Tracing Collaborative Example: Contact Tracing Script COVID-19 Community Tracing Collaborative Media and Outreach Approach A National COVID-19 Surveillance System: Achieving Containment COVID Act Now COVID-19 Tracker Thresholds States Must Meet To Control Coronavirus Spread and Safely Reopen Evaluating and Testing Persons for Coronavirus Disease 2019 (COVID-19)Slowing and limiting transmission within a community is central to reducing the near-term human cost of the outbreak and ensuring that hospitals will be able to maintain lifesaving and life sustaining care. It can also be highly disruptive, as social distancing measures must become more aggressive in proportion to the exponential spread of the virus. Determinations on the best means of limiting transmission should follow national and state guidance, in addition to considering local risk factors. In general, distancing practices during the early phases of an outbreak should be calibrated to be more aggressive than what observable local conditions might intuitively suggest. Once transmission rates within the community have decreased and the burden on the healthcare system has stabilized or declined, it will become possible to consider incrementally relaxing the range of distancing measures put in place. To avoid increases in community transmission following the lifting of social distancing measures, the “re-opening” of communities must be done in a phased manner with communities achieving specific sets of criteria before moving to the next phase. See below for definitions for the phases of incremental lifting of social distancing measures as well as criteria that should be met before progressing to the next phase of re-opening.
- Clearly outline local social distancing guidelines to the community, implement, and maintain them
- Establish criteria for essential and non-essential activities
- Assess and mitigate secondary impact of social distancing measures
- Develop plans for gradually relaxing social distancing efforts when criteria are met
- Does the community have defined thresholds for when to impose or lift measures for social distancing, including stay-at-home orders, non-essential business closures, and curfews? [1] [2]
- Has community leadership issued guidance on self-isolation and quarantine, including how, when, and where to seek help?
[3]
- Have standards for quarantine and isolation release been established and communicated?
- Have small businesses and corporations been engaged as partners in the response effort?
[4]
- Have concerns about providing paid sick leave and/or work from home policies to discourage disease spread?
- Has messaging with businesses been coordinated in the area regarding measures to slow spread in the community?
- Is there a plan to exclude employees with high-risk exposures from work or mitigate transmission potential if allowed to return to duty?
- Has school leadership (public and private) been engaged on the following:
[5]
- Establishing clear criteria for when to recommend cancelling schools and for how long?
- Maintaining clear and open lines of communication with school and district leadership?
- Developing and testing remote teaching and learning methods in case they are needed?
- Putting mechanisms in place to care for children who need additional resources and to incentivize all children to stay at home, if school is cancelled?
- Providing low-income families with meals?
- Addressing similar requirements for cancellations of aftercare and extracurricular activities provided by the school(s) or district(s)?
- Is there a plan to incentivize interventions that can slow community spread of disease?
- Is there a process in place for addressing noncompliance (e.g., fines, criminal charges, etc.)?
- Does the EOC have a list of all upcoming major conferences, sporting events, concerts, rallies, or other events where large numbers of people may gather?
[6]
- Has the community established guidance criteria or official limitations on gatherings consistent with current public health guidance (as of this date it is 10 people or above)?
- Have health officials conducted a risk assessment for these events?
- Have community leaders encouraged the public to adhere to best practices to reduce transmission including:
[7]
- Proper hand washing?
- Avoiding close contact?
- Staying home if sick?
- Covering coughs and sneezes?
- Wearing face coverings in public?
- Cleaning and disinfecting?
- Once community transmission begins to sustainably decrease, is there a plan for reopening and reintegrating the community following the relaxation of stay-at-home orders? Does the plan consider the criteria and phasing approach recommended in this guide?
- Have the steps to manage future community transmission events been identified?
[8]
- What resources are available for expanding health care and/or fortifying the health care system?
- What sort of plans and procedures can be put in place to prevent diseases from spreading in the community?
- Has the community convened an accounting of lessons learned, pulling in the various sectors that were involved or should have been involved? This could include public and private entities.
- Are key community, civil society, business, and religious leaders regularly engaged to promote active cooperation and incentivize compliance with social distancing measures?
- If a state of emergency has been declared, does the community have plans in place to enforce curfews, quarantines, goods rationing, and other measures while protecting the well-being of the public to the greatest extent possible?
- Is there a specific mechanism for engaging public safety sector to assist, incentivize or enforce social distancing if necessary?
- Does the community have plans in place to ensure essential services continue in the event of a large number of absences?
- Have utility providers, transportation managers, waste management, and other critical infrastructure been engaged? [9]
- Have plans been put in place to ensure that other critical infrastructure continues to operate?
PRIORITY ACTIONS
OPERATIONAL REQUIREMENTS
RESOURCES
Non-Pharmaceutical Interventions (NPIs): Actions to Limit the Spread of the Pandemic in Your Municipality (PAHO) National coronavirus response: A road map to reopening Social Distancing, Quarantine, and Isolation: Keep Your Distance to Slow the Spread Interim Guidance for Businesses and Employers to Plan and Respond to Coronavirus Disease 2019 (COVID-19) Interim Guidance for Administrators of US K-12 Schools and Child Care Programs Get Your Mass Gatherings and Large Community Events Ready (CDC) Prevent Getting Sick (CDC) Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission (CDC) Guidance on the Essential Critical Infrastructure Workforce (DHS) Information about Social Distancing (SCVHHS Public Health Department) Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission (CDC) Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza (WHO) Community Mitigation Framework (CDC) Guidance for School Settings (CDC) White House Guidelines (As of 16 March 2020)COVID-19 poses extreme risks to older populations and those with complicating health conditions. Each local context is unique and each local EOC should create a commonly agreed upon and regularly reassessed list of particularly vulnerable populations and sites (examples included below). Attention must be paid to the needs of these populations and the facilities where they may reside or gather. Reducing transmission among these groups through targeted support measures can help protect them, while also alleviating pressure on healthcare systems.
- Establish a comprehensive list of facilities that house high-risk populations (assisted living facilities, seniors’ communities, prisons, detention centers, etc.)
- Assess facilities’ infection prevention and hygiene practices and supply needs
- Address identified vulnerabilities (PPE, training, infection control practices, visitors, staffing levels, etc.)
- Establish guidance to minimize exposure of high risk groups (such as limiting outside visit to high-risk facilities)
- Focus on the particular needs of marginalized populations, including the homeless and undocumented migrants
- Has a comprehensive list been compiled of high-risk populations and sites where they congregate, including:
- Homeless populations? [1] [2]
- Long-term care facilities?
- Other elder homes and communities? [3]
- Home-care resources?
- Prisons? [4]
- Shelters?
- Places of worship? [5]
- Undocumented populations? [6] [7]
- Other high-density housing where high-risk populations may reside?
- Have those facilities’ infection prevention and hygiene practices been assessed and verified?
- Do these facilities currently have the capacity and appropriate protocol for timely reporting infectious diseases?
- Have high-risk facilities received guidance and site-visits to ensure compliance with policies for infection prevention, to include sufficient access to PPE?
- Have regulatory authorities been involved in the assessments of these facilities?
- Has visitor access been restricted to facilities with high-risk groups?
- Are there additional strategies to protect the safety and well-being of high-risk and underserved populations?
- Have you been in contact with regulatory authorities for these facilities?
- Are high-risk populations able to access support while self-quarantined?
- In vulnerable facilities where confirmed cases were identified have procedures been developed for disinfecting and have standards been established for reopening these facilities?
PRIORITY ACTIONS
OPERATIONAL REQUIREMENTS
RESOURCES
Community Solutions – Homeless Populations Interim Guidance for Homeless Shelters (CDC) Guidance for Community Mitigation- Including information on nursing and long-term care facilities (CDC) Preparedness, prevention and control of COVID-19 in prisons and other places of detention (2020) Practical considerations and recommendations for religious leaders and faith-based communities in the context of COVID-19 Handbook for public health capacity-building at ground crossings and cross-border collaboration Coronavirus disease (COVID-19) technical guidance: Humanitarian operations, camps and other fragile settings Reproductive Health in Crisis Situations Q&A on COVID-19, HIV and antiretrovirals (WHO) Quick Reference for the Minimum Initial Service Package (MISP) for Sexual and Reproductive Health (SRH) Strategic Considerations for Mitigating the Impact of COVID-19 on Key Population-Focused HIV Programs Rights in the time of COVID-19 — Lessons from HIV for an effective, community-led response Preparedness, prevention and control of COVID-19 in prisons and other places of detention (2020) COVID-19 HIV Prevention, Treatment, Care and Support for People who Use Drugs and are in Prisons Prisons and custodial settings are part of a comprehensive response to COVID-19 Handbook for public health capacity-building at ground crossings and cross-border collaboration Coronavirus disease (COVID-19) technical guidance: Humanitarian operations, camps and other fragile settings Management of ill travelers at Points of Entry (international airports, seaports, and ground crossings) in the context of COVID-19 The Lives and Livelihoods of Many in the LGBTQ Community are at Risk Amidst COVID-19 Crisis How to use WHO risk assessment and mitigation checklist for Mass Gatherings in the context of COVID-19 Practical considerations and recommendations for religious leaders and faith-based communities in the context of COVID-19 Mental health and psychosocial considerations during the COVID-19 outbreakKEY OBJECTIVE #5
Reinforce and expand health system surge capacity to sustain healthcare operations and avoid high mortality
The mortality risk posed by COVID-19 can grow substantially if a health system becomes overwhelmed with critical cases. . Experiences from China, Italy, New York, and elsewhere have demonstrated that COVID-19 cases can overwhelm health facilities and crowd out other critical medical needs. Identifying creative means of surging overall medical capacity as well as expanding critical care capacity will be urgent as case counts grow. Urgent action should be taken to minimize the risk of transmission within health settings (nosocomial transmission). Telehealth consultations, including the use of telemedicine oversight of critically ill patients in the emergency department and intensive care units, should be considered as an option to triage cases as well as manage patient care.
- Track hospital occupancy rates (overall and critical care) in real time and project future occupancy requirements based on trend
- Ensure hospitals have activated emergency plans and initiated measures to reduce elective or non-urgent medical activities
- Track PPE availability at critical facilities
- Identify alternate PPE purchasing and manufacturing sources
- Initiate plans for surge expansion of critical treatment capacity
- Work with health officials to establish clear criteria to prioritize patients for care and establish referral systems for severe cases
- Initiate plans to separate screening and intake of potential COVID-19 cases from general health care intake
- Track exposure and infections of health workers and assess impact on system capacity
- Initiate plans to screen employees daily for signs and symptoms of illness
- Establish daily operational communication to discuss current case volume (suspected and confirmed), assess hospital census, and staffing needs
- Are healthcare facilities in the community able to provide care to all those who need it?
[1]
- Is there a process in place to continually assess the level of demand on hospitals and understand the risk of those facilities becoming overwhelmed? Does this process feed into a state or federal plan to access and allocate PPE to your community? Are there alternate, quality-controlled, procurement or manufacturing options available (see resources below)?
- Do your local healthcare facilities have a current emergency operations plans and has it been shared with the EOC?
- Do healthcare and EMS providers in your area have sufficient PPE on hand to meet immediate needs? Projected needs?
- Are telehealth capabilities available and supported by internet connections?
- Following laboratory-confirmation of SARS-CoV-2 (COVID-19) in patients or employees, has an exposure and contact-tracing review been performed? Have those exposed been notified and have employees with high-risk exposures been considered for exclusion from work for 14 days?
[2]
- Are priority testing capabilities available for healthcare workers?
- Have alternate sites of care been established with surge capabilities for five to ten times the normal number of pneumonia and influenza admissions at peak flu season? [3]
- Have facilities rescheduled and reprioritized non-emergency care?
- Have treatment centers established separate triage lines for patients with influenza-like illness and/or upper respiratory infection?
- Are specific plans in place to:
- Expand critical care/ICU capacity/extracorporeal membrane oxygenation, including additional ventilator capacity?
- Provide prescription medications for two to three months for all patients, eliminating co-pay penalties and insurance restrictions?
- Offer mail-order or other remote refill mechanisms?
- Triage patients to preserve hospital resources for those most acutely ill?
- Utilize the electronic medical record system for proactive infection control measures such as triggers for isolation precautions based off screening questions or tests being performed?
- Cohort inpatient units for suspected or confirmed COVID-19 patients?
- Govern crisis standards of care plans focused on the decisions that will govern scarce resource allocation?
- Surge healthcare workforce, including in the event that medical staff are infected?
- Develop processes for emergency credentialing of providers (doctors and nurses)?
- Provide rapid training to bolster medical surge capacity?
- Sustain corpse management, avoid morgue overflow, expedite issuance of death certificates, and meet resource requirements, including medical examiner capacity?
- Safely manage waste?
- Provide wellness and mental health support in times of crisis?
- Provide family support resources to healthcare workers to avoid staff distraction?
- Are facilities continually reassessing:
- Occupancy rates?
- PPE supply and predicted usage rates?
- Critical care capacity?
- Ventilator and oxygen capacity?
- Thresholds for triggering/expanding crisis standards of care plans?
- Do local triage and infection prevention/control protocols reflect the risk from COVID-19?
- Have response protocols been established and implemented for suspect cases and persons under investigation?
[4]
- Do response protocols include steps toward release from isolation or quarantine?
- Are environmental controls in place, such as negative pressure rooms, access-controlled entry points, and sterile processing?
- Have hospitals established relationships with state/local public health labs, commercial labs, and academic reference labs to establish testing protocols?
- Have hospitals established relationships with funeral homes, crematoria, and etc. to manage an anticipated surge in deaths?
- Have facilities put into place measures for critical supplies including:
- Arranging for alternate suppliers?
- Expanding inventories, while avoiding excessive hoarding?
- Centralized inventories to mitigate unnecessary usage?
- Using the conserve, reuse, recycle approach to extend use and re-use of PPE?
- Expanded fit-testing capabilities for N95 respirators?
- Engaging the private sector to assist in supply and logistics chain strengthening?
- Have additional staff been hired and trained (could include leveraging academic medical centers for training and reaching out to volunteer staff, non-practicing health care professionals, or advanced medical and nursing students)?
- Have professionals been cross-trained for out-of-scope-practices (i.e. pharmacists, nurse practitioners, physicians who specialize in less relevant areas)?
- Are there plans to re-purpose non-critical staff to assist with operational tasks?
- Have healthcare facilities developed procedures for disinfecting and reopening the portions of their facilities dedicated to the triaging and care of suspect and confirmed COVID-19 patients?
PRIORITY ACTIONS
OPERATIONAL REQUIREMENTS
RESOURCES
Interim Guidance for Emergency Medical Services (EMS) Systems and 911 Public Safety Answering Points (PSAPs) for COVID-19 in the United States (CDC) Training for Infection Prevention and Control (IPC) for Novel Coronavirus (COVID-19) (WHO) Crisis Standards of Care (TRACIE) Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings Alliance PPE Supplier Spreadsheet USFDA surgical N95 whitelist USFDA KN95 whitelist Strategies for Optimizing the Supply of N95 Respirators World Health Organization Training for Infection Prevention and Control (IPC) for Novel Coronavirus (COVID-19) Crisis Standards of CarePublic officials have an obligation to accurately and transparently relay risk information, even (or perhaps especially) when it is alarming. Community trust can make or break an outbreak response, because the effectiveness of social distancing and other interventions hinges on community compliance. Risk communication should follow best practices to mobilize informed action rather than inducing panic. A set of Critical Information Requirements (CIRs) for leaders/decision makers should be set by an EOC, updated daily, and help feed a set of Public Information Requirements (PIRs) that should be communicated to affected populations in ways that are easily accessible by all.
- Establish a regular briefing rhythm to inform community leaders and members
- Provide balanced and measured information; explicitly communicate uncertainty; do not sugar-coat bad news or over-promise potential progress
- Engage with community, business, religious, and other civil society leaders to equip them to be credible sources of information for their stakeholders
- Is community leadership regularly and effectively communicating with various sectors of your government and non-governmental organizations (policy, education, etc.) to discuss ongoing activities? [1]
- Is community leadership communicating with the people who live and work in your community on a routine basis?
- Have the most effective communication methods been identified?
- Can critical communications reach everyone?
- Is there an emergency alert systems in place and tested?
- Is there an effective way to dispel disinformation or misinformation?
- Have trusted spokespeople been identified and assigned to relay important, fact-based messages to the community? [2]
- Have continuity of communications plans been reviewed for the EOC and first responders in the event that mobile communications are disrupted/crash?
- Has a set of critical information requirements for leaders and decision makers been established? Does it help feed public information requirements easily accessible online?
- Are community engagement efforts specifically reaching peripheral or marginalized populations, including undocumented populations? Are there established and tailored messages and mechanisms for communicating with affected or at-risk populations?
- Are materials available in multiple languages, including American Sign Language and braille-based, and accessible for all populations in your community?
- Is there a strategy in place for designating sources of accurate/timely information, monitoring and addressing people’s perceptions, beliefs, and sources of misinformation or disinformation?
- Have existing emergency coordination and emergency public information structures been activated?
PRIORITY ACTIONS
OPERATIONAL REQUIREMENTS
RESOURCES
Interim US Guidance for Risk Assessment and Public Health Management of Persons with Potential Coronavirus Disease 2019 (COVID-19) Exposures: Geographic Risk and Contacts of Laboratory-confirmed Cases (CDC) COVID-19 Risk Communication Package for Healthcare Facilities (WHO) Guide for Preventing and Addressing Social Stigma Associated with COVID-19 (WHO) Communicating Risk in Public Health Emergencies Communicating Risk in Public Health Emergencies TEPHINET Risk Communication Training Public Health for Mass Gatherings: Key Considerations (WHO)Pandemic outbreaks can cause enormous social and economic disruption. These disruptions are damaging in their own right but can be particularly problematic if they create economic disincentives to cooperating with social distancing measures. Mitigating these disruptions can help to reduce the human cost of the outbreak, beyond the immediate toll of the disease itself. Leaders should also pay careful attention to the impact that both the outbreak itself, and the measures to control it, may have on vulnerable populations.
- Establish mechanisms to address impacts of the pandemic on vulnerable populations (e.g. food insecure families reliant on school lunch programs)
- Assess and mitigate impact of social distancing measures on key workforce sectors (health care, public services, etc.)
- Assess second-order impacts of social distancing measures on the local economy
- Assess impact of business closures on local tax revenues and advocate for state/federal support to ensure continuity of government operations
- Identify and work to mitigate economic disincentives to social distancing measures
- Do you have a strategy in place to ensure medications are available to those that need them? [1]
- In the event of a stay-at-home social distancing order, is the community able to provide the necessary resources (e.g., food, medical care, other necessities) to the affected populations? [2]
- Are there mechanisms in place to support neighborhood food distribution and door-to-door service provision?
[3]
- Are community maps accurate and updated?
- Are there designated sub-sections for door-to-door distribution across the community?
- Are there plans in place to mitigate the challenges of social distancing, quarantine, and/or isolation on at-risk populations?
- Is there a proactive plan for economic recovery following disruptions due to business closures and cancellation/postponements of events?
- Are there plans or procedures to request assistance from other jurisdictions or levels of government to provision essential services if the normal departments become unable to?
- Are mutual aid agreements in force? [4]
- Does the community have plans in place to ensure caregivers are allowed to take time off due to lack of child care if schools/daycares are cancelled, including by providing family care leave?